An overview of disease, diagnosis and treatment
Ovarian cancer includes cancer in the ovaries, fallopian tubes and primary peritoneal cancer.
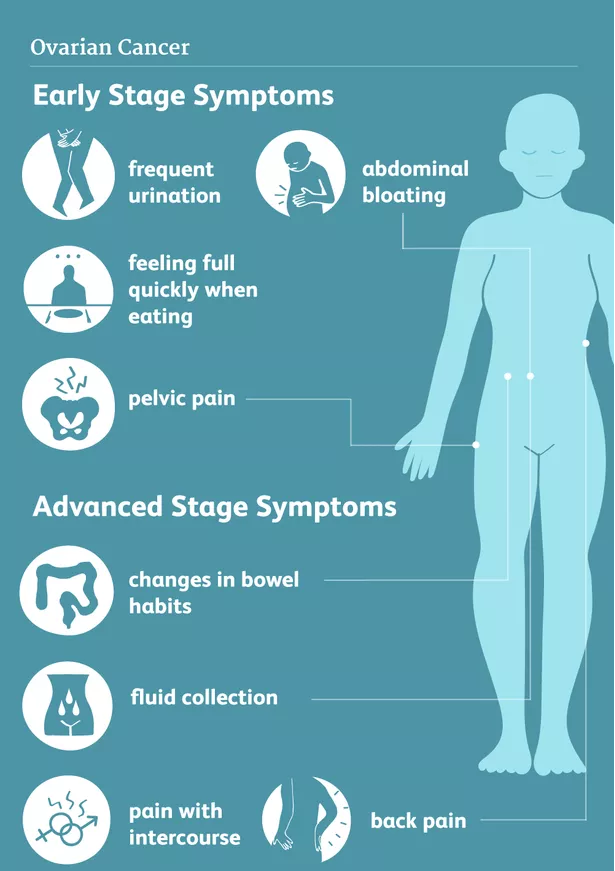
Most tumors arise from the surface (epithelial lining) of these structures and present with few or no symptoms in the lower stages (stage 1-2). The majority of patients have stage 3 or 4 disease (advanced disease) upon diagnosis.
Since the disease has very few or no symptoms initially, many patients have presented with vague or diffuse symptoms to their primary physician, thereby unintentially extending the diagnostic phase.
Epidemiology
Women diagnosed with ovarian cancer are a median age of 63 years, and most are post-menopausal.
The ethiology of the disease is multifactoriel, and approximately 10 % are hereditary (mainly BRCA 1/2 mutation).
As the prognosis is dependent upon stage at diagnosis, and most patients are diagnosed with metastatic disease (stage 3-4), ovarian cancer has a rather poor diagnosis. The 5 year survival rate is above 80 % in stage 1, but 20% in stage 4.
Tumor stage, and whether complete resection of cancerous tissue can be attained at surgery, are the most important factors in terms of long-term prognosis and survival.
Diagnosis
Ovarian cancer is predominantly diagnosed in stage 3 and 4. Symptoms are often unspecific and may include pelvic/abdominal symptoms like discomfort, pain, obstipation, bloating (due to fluid (ascites)), urinary tract irritation/infection, dyspnea, and deep venous thrombosis.
Patients presenting to their primary physician with symptoms indicating ovarian tumor, should be referred for specialized gynaecological evaluation with gynaecological examination, vaginal ultrasound and blood tests incl. the tumor marker Ca-125, which is used for ovarian cancer.
Verification of the diagnosis and histological subtype is required. The gynaecologist will retrieve tumor tissue sample(s) (biopsies) either by ultrasound-guided biopsy, or laparoscopy.
For final staging of ovarian cancer, an imaging examination must be performed to determine the extent of disease. The modality of choice varies between locations between PET/CT, CT, and MRI.
If larger quantities of fluids has accumulated in the abdomen (ascites) or chest (pleural effusion), patients can experience marked abdominal swelling, gastrointestinal irregularities or shortness of breath.
It can be indicated to drain the fluid from the abdomen or chest with a needle (paracentesis or thoracentesis) to alleviate severe symptoms. The extracted fluid may contain cancerous cells, and can be send for histological examination to document the diagnosis, if indicated.
Multi Disciplinary Team (MDT) Conference: When results from abovementioned examinations are available, best advised treatment strategy is discussed between doctors in the Multi Disciplinary Team. If initial surgery (Primary debulking Surgery (PDS)) is deemed technically and medically feasible, this will be recommended initially.
Patients with stage 4 ovarian cancer can start their cancer treatment with chemotherapy. The aim is to decrease the tumor bulk, before undergoing interval surgery later (Interval Debulking Surgery (IDS)).
Examinations
Transvaginal Ultrasound
An ultrasound examination of the internal genital organs is carried out with an ultrasound probe inserted into the vagina (transvaginal sonography). It demonstrates pelvic structures well, but is insufficient to visualize cancerous lesions on e.g. bowel surfaces.
It is painless and can be repeated any number of times. It does not expose the patient to any radiation.
Abdominal Ultrasound
Ultrasound examination of the abdomen provides view of the internal organs such as the liver, kidneys, spleen, and to some degree the intestines. It may visualize, possible tumorspread (metastases) to nearby organs or structures.
The presence of abnormal fluid effusions accumulated in the abdominal cavity (ascites) or in the chest (pleural effusion) can cause debilitating symptoms for the patient.
The size/amount, and exact location of effusions/fluid pools can be determined with ultrasound, and a needle and tube be inserted for drainage and fast symptom relieve. The risk of unintentionally damaging nearby structures is diminshed by ultrasound-guidance during the procedure.
Blood Tests
Blood tests provide information about the general health condition of the patient.
The test results are important with regard to any upcoming treatment, and usually evaluates both haematological status, kidney- and liverfunction, coagulation status and the tumor marker Ca-125.
Tumor markers are of particular use for monitoring the course of the disease during chemotherapy, and in the event of a relapse. In the post-treatment phase, a rise in level of tumor marker can be an indicator of relapse.
Treatment options
Chemotherapy
For patients who undergo primary debulking surgery: Based on the stage, histological type, surgical findings and outcome, the recommendation/option of receiving post-surgical treatment with “adjuvant” chemotherapy will be discussed with you. Only for certain malignant ovarian tumors in stage 1, surgical treatment is deemed sufficient, and omitting “adjuvant” chemotherapy is advised.
For patients who undergo interval debulking surgery: To reduce the tumor bulk before surgical removal of the remaining tumor, patients will be treated with “neoadjuvant” chemotherapy. Here 3 series (rounds) of combination chemotherapy is given, followed by new imaging and blood sample evaluation of the tumor response. If deemed surgically and medically feasible, patients will undergo surgical resection af remaining tumor.
Chemotherapy are powerful pharmaceutical drugs used to destroy/kill cancer cells throughout the body. The drugs work by inhibiting cell growth, thereby aiming to induce tumor regression.
The standard option for ovarian cancer is a combination chemotherapy with two drugs (carboplatin and paclitaxel/docetaxel), which are given 6 times with 3 weeks apart.
In advanced stages (stage 3 & 4) the antibody bevacizumab or a parp inhibitor can be administered during/following the chemotherapy according to guidelines. The intention is to extend the time until relapse.
What are the side effects of chemotherapy?
Treatment with chemotherapy also affects normal tissue, which can cause side effects. Especially tissues which renew themselves quickly, are likely to be affected. These include the mucous membranes of the mouth, stomach and intestines, the hematopoietic system in the bone marrow, and the hair roots. Several side effects can be alleviated well with medication, and usually disappear/diminishes significantly, when chemotherapy is no longer administered.
Surgery
Patients are operated for ovarian cancer under general anesthesia. It is a complex and large procedure performed by specialized oncological surgeons in gynaecologic surgical departments. A longitudinal abdominal incision is made during the operation.
The aim of the operation is to completely remove all tumor tissue, which involves removing both ovaries, fallopian tubes, the uterus, the abdominal fatty network, appendix, and parts of the peritoneum and lymph nodes. The size of the operation depends on the extent of invasion and type of the tumor. Sometimes parts of the intestine are removed also, and a stoma can be necessary to accomplish surgical radicality.
In selected cases, where only one ovary is affected (stage 1) in fertile women, fertility-preserving surgery may be considered.
AntiBody Therapy And PARP-Inhibitors
Research demonstrated, that adding the anti-angiogenesis antibody bevacizumab to the chemotherapy regimen, can considerably extend the time to relapse of cancer. Bevacizumab treatment is referred to as “targeted therapy”. Via binding to the VEGF-receptor in patients, bevacizumab inhibits the formation of new blood vessels, thereby reducing the blood supply to the tumor. (OCEANS, GOG-213 studies)
Important clinical studies demonstrated significant effect of PARP-inhibitor maintenance treatment on progression free survival following platinum-based chemotherapy in ovarian cancer patients. Patients with BRCA 1/2 mutation and/or HRD have the highest degree of effect of PARP-inhibitor maintenance. (NEJM, 2019, PRIMA, PAOLA studies).
In Case Of A Relapse
Despite initial surgery and chemotherapy success, many patients experience relapse of the cancer. The treatment approach will in each case be evaluated thorougly, to determine best possible options.
In most cases relapsed disease is not curable. The treatment focuses on preventing tumor growth and further spread of metastases for as long as possible, thereby relieving symptoms and hopefully prolonging duration of good quality of life.
Depending on how fast, and in which form, the tumor relapse occurs, an additional surgical procedure may be advised, followed by a subsequent new round of chemotherapy.
If relapse occurs within half a year after initial surgery and completion of the first line of chemotherapy, the choice of next chemotherapy will typically be pegylated liposomal doxorubicin. For further future relapses or progressions paclitaxel or other drugs may be administered.
Inclusion in ongoing clinical trials in your oncological department may also be possible. Participation in a clinical trial can in some cases have a direct impact on your quality of life and/or your prognosis. However, in other cases the study will mainly benefit future patients. Ask you treating dorctor(s) about your possibilities and options.
Making Decisions About Your Care
The choice of therapy for your cancer is an individual decision, and many factors are taken in to consideration, when your doctor(s) discuss the best option(s) with you. These include the type, size and location/spread of the tumor, as well as your age and general health status.
We recommend, that you have a thorough discussion with your doctor(s) about the results upon your diagnosis, the treatment-plan and your chances of recovery (e.g. prognosis).
You are encouraged to include family and/or friends for participation in doctors appointments etc. for improving your/their understanding and remembrance of relevant information, as well as for emotional and physical support during appointments and treatments.
Your doctor can give a detailed explanation of the various therapy options, and has knowledge of the possibility to participate in a clinical trial. Each patient is different and so is their wish upon information needed/wanted prior to making important decisions.
Well designed and conducted clinical trials are essential to determine the effectiveness of a promising new drug or intervention. Many gynaecologic oncology departments have studies open for inclusion during the course of your cancer treatment. Talk to your doctor(s) about your thoughts regarding possible inclusion in a clinical trial now or in the future.
Author: Kristine Madsen, MD, Medical Director NSGO-CTU