An overview of disease, diagnosis and treatment
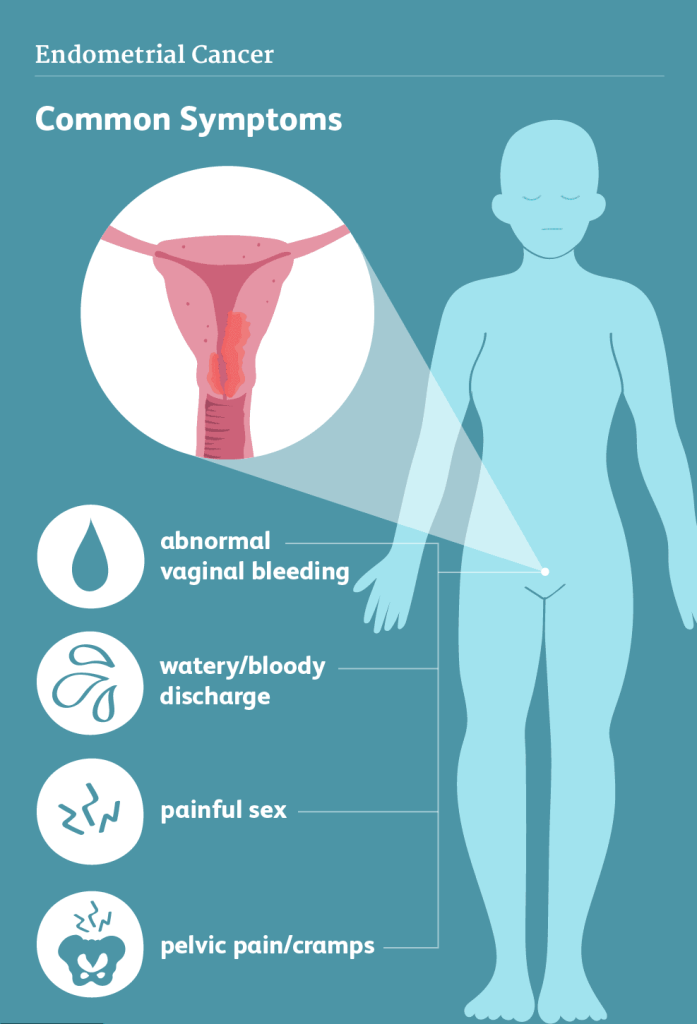
The uterus is the pelvic, hollow, pear-shaped female reproductive organ, where fetal development occurs. In later stages of life, it is also the location of the most common gynaecological form of cancer. Cancer of the uterine body mainly originates in the internal uterine lining (endometrium), and is therefor also referred to as endometrial cancer. Endometrial cancer is often detected at an early stage, as it frequently causes abnormal and/or post-menopausal vaginal bleeding. If endometrial cancer is discovered early, surgical removal of the uterus can cure the disease.
Epidemiology
Women diagnosed with endometrial cancer are a median of 69 years, and most patients are postmenopausal.
High levels of estrogen in women predispose to development of endometrial cancer and include adipositas, PCOS, diabetes mellitus, tamoxifen (used in breast cancer treatment), and hormone replacement therapy (HRT).
The prognosis is good in stage 1 with more than 90 % being alive after 5 years. In stage 3 the 5 year survival rate is 40 %.
Diagnosis
Endometrial cancers tend to give symptoms early on. Patients may present to their doctors with irregular vaginal discharge/bleeding (e.g. on/after hormone (estrogen) treatment), or with post-menopausal bleeding. Later on discomfort, pain and urinary tract irritation/infection may arise.
Theses patients will be referred for specialized gynecological evaluation, where initially a gynaecological examination, vaginal ultrasound, and blood tests are performed.
Tumors may present as papillary (extending into the cavity), or more profound growing in the uterine wall. Tissue must be extracted from the tumor for histological examination to make a final diagnosis. This is done via a hysteroscopy or by endometrial fractional abrasion during gyneacological examination.
For staging of endometrial cancer an imaging examination must be performed to determine the extent of disease. The modality of imaging varies between locations between PET/CT, CT, and MRI.
Examinations
Transvaginal Ultrasound
An ultrasound examination of the internal genital organs is carried out with an ultrasound probe inserted into the vagina (transvaginal sonography). It demonstrates pelvic structures well, but is insufficient to visualize cancerous lesions on e.g. bowel surfaces.
It is painless and can be repeated any number of times. It does not expose the patient to any radiation.
Hysteroscopy
During a hysteroscopy a thin, flexible, lighted tube (hysteroscope), is inserted through the vagina and cervical canal into the uterine cavity. With a lens on the hysteroscope the examiner can oversee the hollow internal cavity and lining of the uterus. In case of suspicious areas, tissue samples are taken and send to the pathologists for histological examination. The uterus examination is usually combined with scraping of cells from the lining (fractional abrasion).
Curettage (abrasion/Scraping Of The Endometrium)
Obtaining tissue samples from suspicious areas in the endometrium is necessary to detect malignant lesions in the uterus, and thereby make a final histological diagnosis.
Tissue samples from the uterine and cervical canal membranes are carefully obtained by scraping, and the samples are collected for examination. It can cause minor discomfort and bleeding for a few days, but then the mucous membranes gradually rebuild again.
Blood Tests
These tests provide information on the general health condition of the patient. Doctors may examine blood tests for hemathological status, renal-, and liverfunction as well as the ability to coagulate their blood during/after surgery.
No tumor marker is available for diagnosing/follow up on patients with endometrial cancer.
Treatment options
Surgery
The first choice of treatment for patients with endometrial cancer is surgery, if this is deemed feasible by the specialized oncological gynaecology team.
The uterine body is removed along with the fallopian tubes and ovaries. The operation aims to remove all tumor tissue and any cancerous lymph nodes in the pelvis and abdomen. If there are involvement/spread to neighboring organs (such as the bladder and rectum), theses may also be removed in selected cases. Many patients in lower stages (1-2) are cured by the surgical procedure alone.
The operation can be performed with an abdominal incision, or in early stages by hysteroscopic surgery.
All removed tissue is send for pathological examination for determination of final cancer type, grade, and stage of disease.
This information is essential for determining, if oncologic treatment is warranted also.
In certain cases with advanced stages, the surgical procedure is accompanied with radiation and/or chemotherapy. The aim is to destroy/kill any remaining cancer cells in the body, thereby reducing the risk of relapse of cancer.
Patients may experience complications or side effects after the surgery. In general the greater the procedure, the higher risk of complications such as e.g. hardened scar/fibrous tissue, lesion/dysfunction of nearby structures/organs, fluid gathering in the underlying tissue or legs (lymphoedema), sexual complaints etc. We recommend you discuss these issues with your doctor(s).
Chemotherapy
For patients who undergo primary surgery: Based on the stage, histological type, surgical findings and outcome, the recommendation/option of receiving post-surgical treatment with “adjuvant” chemotherapy will be discussed with you. It will be recommended to give adjuvant chemotherapy for a selected group of patients with high risk disease based upon stage and/or histological type and mutational status.
Chemotherapy are powerful pharmaceutical drugs used to kill fast-growing cells (e.g. cancer cells) throughout the body. The drugs work by inhibiting cell growth, thereby aiming to induce tumor regression.
The standard adjuvant chemotherapy for endometrial cancer is a combination therapy with two drugs (carboplatin and paclitaxel), which are given intravenously six times with 3 weeks apart.
Treatment with chemotherapy also affects normal tissue, which can cause side effects. Especially tissues which renew themselves quickly, are likely to be affected. These include the mucous membranes of the mouth, stomach and intestines, the hematopoietic system in the bone marrow, and the hair roots. Several side effects can be alleviated well with medication, and usually disappear/diminishes significantly, when chemotherapy is no longer administered.
Endocrine Therapy
Anti-hormonal therapy (endocrine therapy) can be used for patients with recurrent/disseminated endometrial cancer, if metastases (daughter tumors) have spread to other locations or organs in the body. Endocrine therapy has significantly fewer side effects than chemotherapy. The effect of hormone therapy is slower in onset, than that of chemotherapy. Chemotherapy is usually given initially as treatment for metastatic disaese with signinficant/severe symptoms incl. shortness of breath due to spread to the lungs.
Fragile and/or elderly patients who may not be candidates for (further) chemotherapy do in many cases tolerate endocrine treatment well. Some patients derive benefit from the treatment for extended periods of time.
Particularly aggressive, malignant tumors usually do not respond well or at all to endocrine therapy.
Anti-hormone treatment can have side effects, such as weight gain, nausea, dry skin, and sleep-disturbances. The side effects disappear after the therapy stops, and are overall less disturbing, than those caused by chemotherapy or radiation treatment.
Radiation Therapy
For more advanced cancers (at diagnosis), a combination of surgery with radiation and/or chemotherapy may be recommended.
The radiation therapy is given to a limited part of the pelvic area, and is effective and intended to reduce the risk of relapse (adjuvant radiation therapy).
Radiation therapy kills or destroys any remaining malignant cells after surgery. Radiation may be given from the outside (external), or through the vagina (internal). Ask your doctor about the recommendations for your specific case.
In several countries radiotherapy is not given routinely in combination with surgery and chemotherapy due to the risk of persistent side effects. There radiotherapy is reserved for selected high risk cases, and for patients with localized relapse in the pelvis. The treatment can still be curative in nature, if given to correctly selected cases.
The nature and extent of patients physical complaints (side effects), during or following radiotherapy, are often relative to the extent of pre-radiation surgery, and the size of the irradiated field. The more extensive the treatment, the sooner and the more extensive the side effects may be.
Radiation should only be used instead of surgery, if serious health issues are present, which makes surgery too great a risk for the patient.
Making Decisions About Your Care
The choice of therapy for your cancer is an individual decision, and many factors are taken in to consideration, when your doctor(s) discuss the best option(s) with you. These include the type, size and location/spread of the tumor, as well as your age and general health status.
We recommend, that you have a thorough discussion with your doctor(s) about the results upon your diagnosis, the treatment-plan and your chances of recovery (e.g. prognosis).
You are encouraged to include family and/or friends for participation in doctors appointments etc. for improving your/their understanding and remembrance of relevant information, as well as for emotional and physical support during appointments and treatments.
Your doctor can give a detailed explanation of the various therapy options, and has knowledge of the possibility to participate in a clinical trial. Each patient is different and so is their wish upon information needed/wanted prior to making important decisions.
Well designed and conducted clinical trials are essential to determine the effectiveness of a promising new drug or intervention. Many gynaecologic oncology departments have studies open for inclusion during the course of your cancer treatment. Talk to your doctor(s) about your thoughts regarding possible inclusion in a clinical trial now or in the future.
Author: Kristine Madsen, MD, Medical Director NSGO-CTU